By Jonathan G. Wiik, Vice President, Health Insights, FinThrive
New year, new data! While the numbers from the end of 2022 continue to show the same challenges faced throughout the year – negative margins, staffing issues, inflation, unpredictable volumes – there is hope on the horizon. Recovery seems to be on the way, with projections looking particularly positive for the second half of this year. Let’s see what’s ahead for 2023.

Webinar On Demand
Healthcare in 2023 and beyond — A financial outlook for revenue leaders
Presented by: Jonathan G. Wiik, MSHA, MBA, CHFP, Vice President, Health Insights, FinThrive
Jonathan discusses how successful organizations are using people, process and technology to change healthcare's financial paradigm.
Volumes in 2022 Remained Below Pre-Pandemic Levels
2022 saw volumes stay below pre-pandemic levels in all areas, with the emergency department and inpatient areas most pronounced. Outpatient visits showed some recovery, but still finished 2022 with below normal volumes.
Emergency department, inpatient, and outpatient were -3.8%, -8.7% and -11.5% respectively, as seen in the graph below. Compared to 2021, 2022 experienced 15.4% less volume at hospitals overall, with -12% less in emergency department, -19% less in inpatient, and -15% less in outpatient.
We anticipate that 2023 will likely continue to experience subpar volumes into Q1 as hospitals struggle to climb out of labor and supply/inflation constraints. Volumes should recover to single-digit deficits into Q2 for inpatient and emergency department visits, and outpatient visits may break even or have a slight surplus as the year progresses. This will hinge on the “tri-demic” impacts to hospital operations, inflation, and the market’s ability to stabilize staffing and operate at full capacity.
Weekly Visit Volumes by Treatment Setting
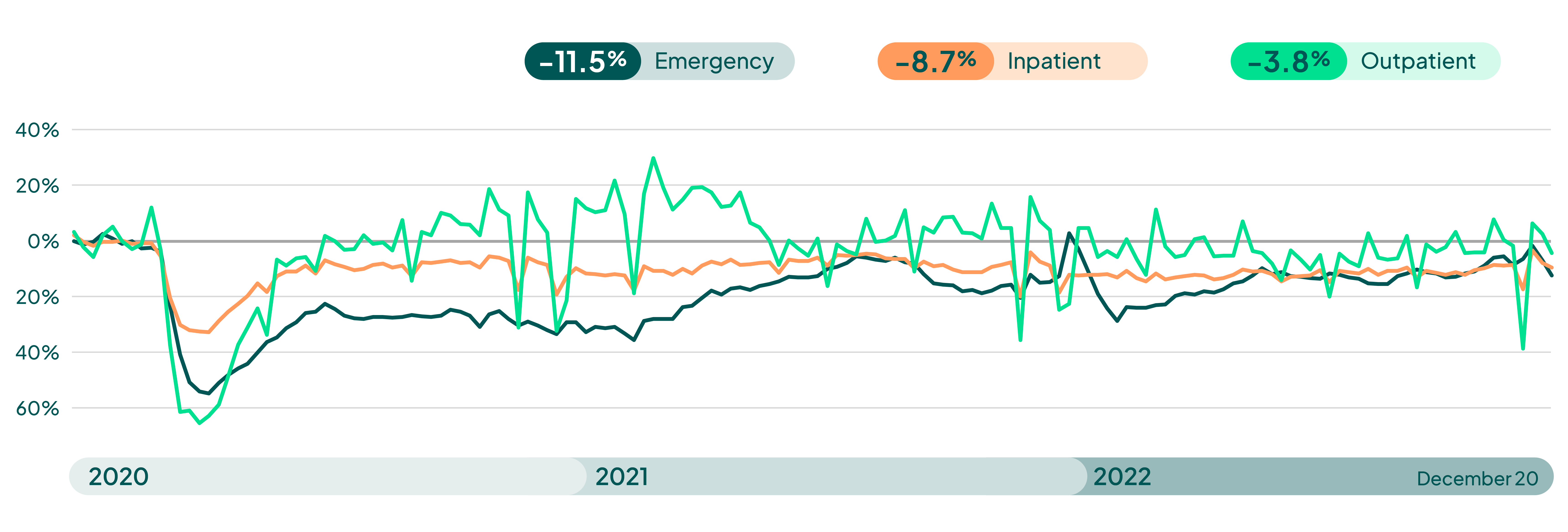
Source: FinThrive Proprietary Data (n=500 hospitals)
December’s Kaufman Hall National Hospital Flash Report revealed negative margins for all of 2022 thus far (11 months total as of Nov. ‘22). Although the industry has seen some financial recovery, it remains in a deficit driven by headwinds from subpar volumes, labor and supply expense, as well as fragile payer relations. The report details YOY performance in margin, revenue, expenses, and volumes at the regional level, and highlighted four key takeaways:
- Margins: Margins remained negative for 11 out of the 12 months of 2022, but with steady improvement.
- Expenses: Expenses cooled for hospitals in November, with ALOS and other key volume metrics declining, resulting in improved margins for November.
- Labor: Labor, which has plagued the industry for most of the year, is starting to see some recovery. Labor expense decreased through less reliance on contract labor.
- Volumes: Outpatient revenue is recovering as well and can help to buoy margins into 2023, as we see deficits in emergency and inpatient visits.
Operating Margin Index by Month
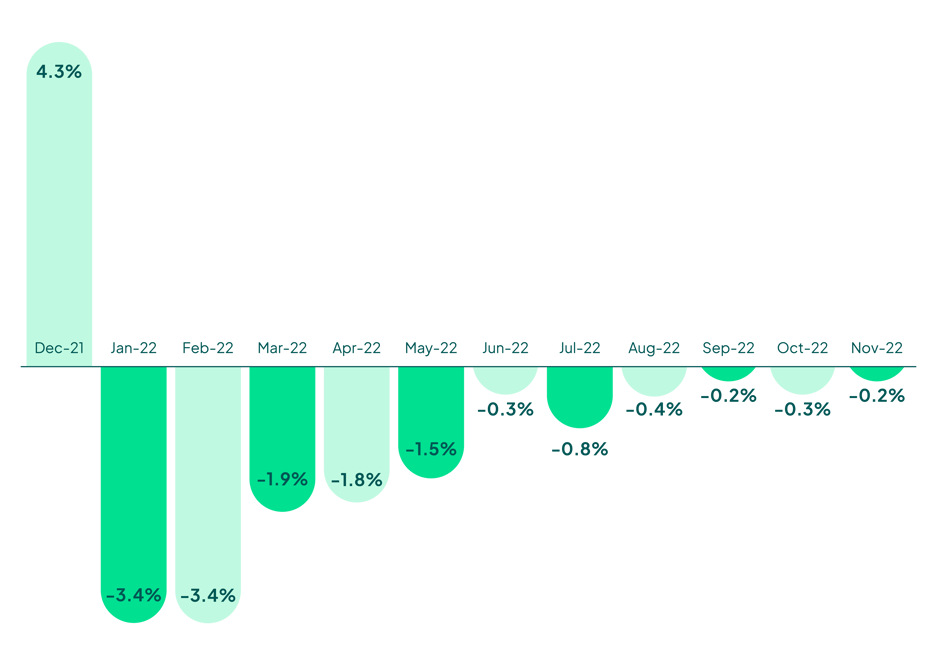
Source: Kaufman Hall December 2022 National Hospital Flash Report
Expenses and Volumes
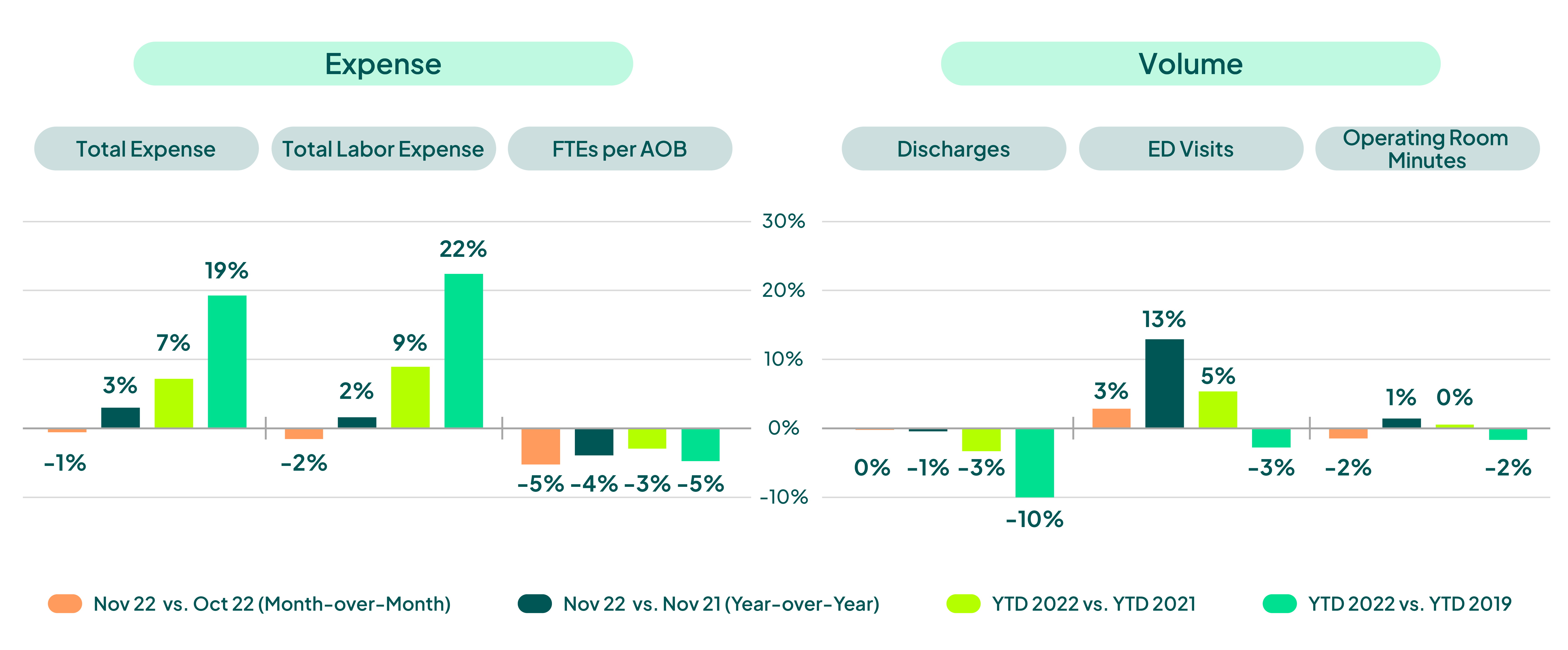
Source: Kaufman Hall December 2022 National Hospital Flash Report
Impacts
Hospital admissions have surpassed the spike seen in July of last year and are now above 40K COVID-19 inpatients. This represents approximately 7% of a hospital’s overall IP (med/surg) and ICU capacity per HHS reporting. For reference, during Omicron, these thresholds were in the 15% - 35% range.
The “Tri-demic” may have some material impact in hot spot areas where beds are limited; however, the overall impact to hospital operations should be immaterial for now. Some leveling should occur here as the downslope of flu season is coming, and CDC is already reporting this downward trend.
Earlier this month, HHS renewed the Public Health Emergency another 90 days into April. However, that will likely soon be changing: the latest $1.66T Omnibus package affords states the ability to start the redetermination process for Medicaid in April, even with the PHE in place. This will likely lead to the disruption of 15M+ Medicaid beneficiaries per ASPE. This will impact a little less than 1 in 5 Medicaid beneficiaries and will have material impact on hospital uncompensated care.
Congress has already rung the bell pleading HHS to provide more support for hospitals given the 2022 deficit and this looming disruption. Hospitals will need to ramp up resources, address disruption, and ensure care avenues are not blocked due to access and coverage concerns. Organizations should closely examine coverage disruptions, specifically in the Medicaid and Health Benefit Exchange coverage areas. Hospitals can expect higher levels of self-pay and patient bad debt risk as disruptions in coverage occur if/when the PHE expires. It will be imperative to ensure the cash position of organizations is insulated to offset top line revenue risks from lost coverage.
Keys to Recovery
Hospitals have experienced the worst financial performance in decades. Organizations will need to rethink their revenue management, critically evaluating a digital transformation strategy to automate, apply analytics, and radically change how revenue is captured from patient and payer.
The distraction of margin pressures should not distract from the core reason why we are all here: the patient. Financial sustainability is critical to ensure appropriate levels of care are delivered to the right patient, with the right resources, at the right time. Focusing on staff retention, powered by modern automation, enables employees to be more productive, more engaged, and more satisfied by more value-added work.
Patient retention and attraction strategies will need to hinge on frictionless onboarding and intake efforts and patient-friendly billing. Line-of-sight financial clearance and revenue integrity from all funding mechanisms will be a key differentiator for successful organizations. A keen focus on expense and spend as well as looking to partners that consistently demonstrate value will also ensure financial viability going forward. Rethink your revenue management strategy in 2023 by consolidating your footprint of solutions to those that can deliver for your patients and payers.
Note From the Author
The latest data gives us room for optimism – but that doesn’t mean we can be complacent. To accelerate and capitalize on this year’s recovery, organizations must embrace technology, evolve their processes, and leave the “bad old days” of outdated revenue management behind us.
Want to learn more? Request a demo or catch my upcoming webinar with Becker’s Healthcare, Healthcare in 2023 and beyond — A financial outlook for revenue leaders.

About the Author
Jonathan G. Wiik, MSHA, MBA, CHFP
Vice President, Health Insights
Jonathan Wiik, VP of Health Insights at FinThrive, has over 25 years of healthcare experience in acute care, health IT and insurance settings. He started his career as a hospital transporter and served in clinical operations, patient access, billing, case management and many other roles at a large not-for-profit acute care hospital and prominent commercial payer before serving as Chief Revenue Officer. Wiik works closely with the market and hospitals on industry best practices for revenue management. He is considered an expert in the industry for healthcare finance, legislation, revenue management and strategic transformation.








