Cracking the Denials Code:
Enhance Healthcare Financial Performance
Healthcare finance leaders serve as a cornerstone within their organizations and they are equipped to identify what’s working well, invest in technology and set goals to improve financial performance across the revenue cycle.
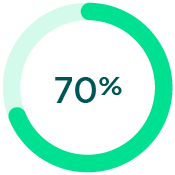
According to FinThrive’s 2024 RCM Transformative Trends Report, which surveyed 92 healthcare finance executives, 70% said increasing revenue was their top goal this year.
But what strategies need to be implemented to capture every dollar?
Healthcare leaders say it starts with denials.
76%
said reducing denials was the top planned initiative
67%
indicated the need to improve the prior authorization process – a common source of denials
36%
stated improving the patient payment experience was a factor
Now, let’s look at the “why” behind the denials conundrum in healthcare.
With every passing year, denials seemingly become a bigger thorn in the sides of providers and patients.
The reason? Payers are playing hardball.
The burden is only getting heavier for hospitals and health systems
97%
report patients experienced delays or denials for medically necessary care due to prior authorization requirements1
95%
report increases in staff time seeking prior authorization approval2
84%
say the cost of complying with insurer policies is increasing3
78%
indicated that their experience with commercial insurers is getting worse4
Denials also impact healthcare organizations’ bottom lines
$1.6M
in denial write-off adjustments
(mid-sized $350M NPR hospital)5
7-11%
of claims are underpaid6
Denial write-offs are only getting worse
4X
Since 2018, denials have increased four times7
<1% NPR
Industry best practice benchmark
4.6% NPR
Current average write-off percentage
So what can providers do to bend the denials curve?
Here are six ways to address some of the most common denials.
![]()
Inaccurate or Insufficient Documentation
Problem:Incomplete patient information, missing signatures and illegible paperwork can lead to claim rejection
Solution:Verify information during pre-service withdigital registration and patient scheduling solutions


![]()
Prior Authorizations
Problem:Disconnection or miscommunication between providers and payers makes it difficult to obtain necessary authorization prior to care
Solution:Streamline authorization processes with electronic, real-time solutions that facilitate better communication with payers
![]()
Coding Errors
Problem: Mismatched diagnosis and procedure codes or incorrect modifiers
Solution: Invest in coding education and training for staff, conduct regular audits and compliance checks to identify and fix coding errors quickly


![]()
Timely Filing Limit Exceeded
Problem: Failure to meet payer deadlines of when claims must be submitted
Solution: Utilize sophisticated claims technology to ensure timely claim submissions
![]()
Insurance Coverage Issues
Problem: Expired policies or services not covered under a patient’s plan
Solution: Verify insurance coverage and eligibility prior to billing with an insurance discovery solution


![]()
Point Solution Overload
Problem: Too many siloed technologies where data is not democratized, analyzed and centralized
Solution: Look to a revenue cycle management platform that offers end-to-end revenue protection across eligibility, claims and revenue integrity
Need a new strategy on how your healthcare organization should prevent or manage denials?
Discover expert strategies to mitigate denials and boost revenue in our comprehensive Denial Management Best Practices Guide.



